Hypoglycemia, often referred to as low blood sugar, is a common and potentially dangerous condition that requires prompt recognition and management. It occurs when blood glucose levels drop below the normal range, leading to various physiological and neurological symptoms. For nurses in India, understanding the nursing diagnosis for hypoglycemia is crucial for timely intervention and patient safety. Proper assessment, accurate diagnosis, and appropriate interventions can prevent complications, improve patient outcomes, and enhance the quality of care. This guide outlines symptoms, nursing interventions, and expected outcomes for effective management.
Assessment and Symptoms of Hypoglycemia
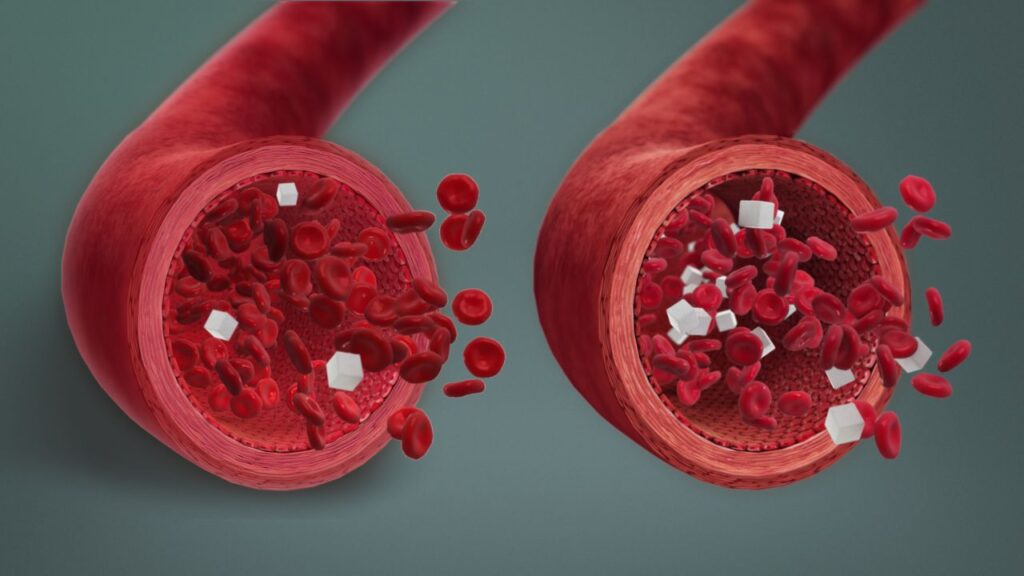
Effective nursing care starts with thorough patient assessment. Key symptoms of hypoglycemia include shakiness, sweating, confusion, irritability, and rapid heartbeat. In severe cases, patients may experience seizures, blurred vision, or loss of consciousness. Nurses should monitor blood glucose levels regularly, especially in patients with diabetes or those receiving insulin therapy. Observing changes in mental status and behavior is essential, as early recognition allows for rapid intervention. Recording the frequency and severity of episodes helps in planning personalized care and educating patients on preventive measures.
Nursing Diagnosis for Hypoglycemia
The primary nursing diagnosis for hypoglycemia focuses on the imbalance between glucose intake and utilization. Commonly used nursing diagnoses include risk for unstable blood glucose, ineffective health management, and risk for injury related to altered mental status. Nurses must identify contributing factors such as medication errors, missed meals, or excessive physical activity. Developing a care plan involves setting realistic short-term and long-term goals to maintain stable glucose levels. Collaboration with dietitians and physicians ensures comprehensive management, including adjustments in insulin doses, dietary planning, and patient education.
Nursing Interventions and Management
Interventions for hypoglycemia aim to restore blood glucose levels and prevent recurrence. Immediate actions include administering oral glucose, juice, or glucose tablets for conscious patients, and intravenous dextrose for severe or unconscious cases. Nurses should continuously monitor vital signs, blood sugar readings, and neurological status. Educating patients on meal planning, regular glucose monitoring, and recognizing warning signs is essential for long-term management. Maintaining detailed documentation of interventions and responses supports ongoing care and provides a basis for evaluating the effectiveness of the nursing plan.
Expected Outcomes and Patient Education
Successful management of hypoglycemia involves achieving stable blood glucose levels and empowering patients through self-care and education. Expected outcomes include improved awareness of hypoglycemia symptoms, adherence to medication and dietary regimens, and reduced frequency of acute episodes. Nurses should provide guidance on emergency measures and follow-up care, ensuring patients know when to seek medical help. Encouraging regular check-ups and lifestyle modifications enhances overall health and minimizes the risk of complications.
| Aspect | Details |
|---|---|
| Common Symptoms | Shakiness, sweating, confusion, irritability, rapid heartbeat |
| Severe Symptoms | Seizures, loss of consciousness, blurred vision |
| Nursing Diagnosis | Risk for unstable blood glucose, ineffective health management, risk for injury |
| Immediate Interventions | Oral glucose, juice, glucose tablets, IV dextrose |
| Long-Term Management | Patient education, dietary planning, regular glucose monitoring |
FAQs
Q1: How quickly should hypoglycemia be treated?
A1: Treatment should be initiated immediately upon symptom recognition.
Q2: Can hypoglycemia occur in non-diabetic patients?
A2: Yes, it can occur due to fasting, illness, or hormonal imbalances.
Q3: What is the first-line intervention for mild hypoglycemia?
A3: Administering oral glucose or carbohydrate-rich food.
Q4: How can nurses prevent hypoglycemia in high-risk patients?
A4: Through regular monitoring, education, and individualized care plans.