Gestational Hypertension NCP: Hey there, future nursing superstar! 🌟 You might have heard of gestational hypertension (GH) before, but do you know how it plays a huge role in the world of nursing? Gestational hypertension isn’t just a fancy term to throw around at medical school—it’s a serious condition that affects pregnant women and needs close monitoring to ensure both mother and baby stay safe. But what does that mean for YOU, as a nursing student? It means you’ll need to be well-prepared to create a comprehensive nursing care plan (NCP) for your patients dealing with this condition.
Thank you for reading this post, don't forget to subscribe!
In this guide, we’re going to break down the essentials of the Gestational Hypertension NCP, taking you through step-by-step how to structure it, the interventions that matter most, and how to measure success. Sounds complicated? Well, trust me, by the end of this, you’ll be an expert at handling this NCP!
Now, let’s start with the basics. Gestational hypertension, also known as pregnancy-induced hypertension (PIH), is when a pregnant woman develops high blood pressure after the 20th week of pregnancy. Unlike preeclampsia (another condition related to hypertension), GH doesn’t always cause protein in the urine or significant damage to organs—but don’t let that fool you. It can still lead to serious complications, like preterm labor, placental abruption, and even stroke.
As a nurse, your job is to catch these early signs, provide the necessary interventions, and ensure that your care plan is in place. Creating a Gestational Hypertension NCP isn’t just about identifying the condition—it’s about responding effectively and monitoring your patient to keep them healthy until the baby arrives.
Let’s dive into it, shall we? 😄
Patient Information: (Example for Learning)
Before we get into the details of the Gestational Hypertension NCP, let’s set up a fictional example to see how it works. Remember, this patient info is completely made up for teaching purposes!
- Name: Priya Sharma
- Age: 28
- Gender: Female
- Medical History: Priya has had a healthy pregnancy so far with no major complications. She has no known history of chronic hypertension or diabetes, but she has been gaining weight rapidly in the last few weeks.
- Symptoms: Priya has been complaining of persistent headaches, visual disturbances (seeing spots), and swelling in her feet. Her blood pressure readings have been higher than usual during her routine check-ups.
- Medical Diagnosis: Gestational Hypertension
- Fever Admission Date: January 15th, 2025
- Care Plan Initiated: January 15th, 2025
This is just an example, but it helps us understand how to approach the NCP for a patient with gestational hypertension.
Comprehensive Nursing Care Plan for Gestational Hypertension
Here’s where we get into the meat and potatoes of your Gestational Hypertension NCP. In this section, we’ll break everything down, and I’ll guide you through how to structure each part of the care plan with ease.
Nursing Assessment: Subjective Data
- Chief Complaint: “I’ve been having headaches and my feet are so swollen! I feel a bit dizzy sometimes, and I can’t sleep very well.”
- History: Priya is in her third trimester and has been feeling unwell for the last week. She denies any past history of hypertension but admits she’s been feeling more stressed lately with work and family.
- Health History: No known chronic illnesses, including hypertension or kidney disease.
- Family History: Priya’s mother had hypertension during pregnancy but didn’t develop preeclampsia.
Objective Data
- Vital Signs:
- Blood Pressure: 155/98 mmHg (higher than normal)
- Heart Rate: 92 bpm
- Respiratory Rate: 18 breaths/min
- Temperature: 98.7°F
- Hydration Status: Mild edema in the lower extremities, signs of water retention.
- Pain Assessment: Priya reports a persistent headache, rated 6/10 on the pain scale.
- Laboratory Values: Blood and urine tests show no protein in urine, but elevated liver enzymes are concerning.
Nursing Diagnoses:
- Risk for Injury related to increased blood pressure and dizziness.
- Impaired Urinary Elimination related to edema and potential renal impairment.
- Risk for Decreased Cardiac Output related to increased blood pressure and swelling.
- Ineffective Health Maintenance related to lack of knowledge on managing hypertension during pregnancy.
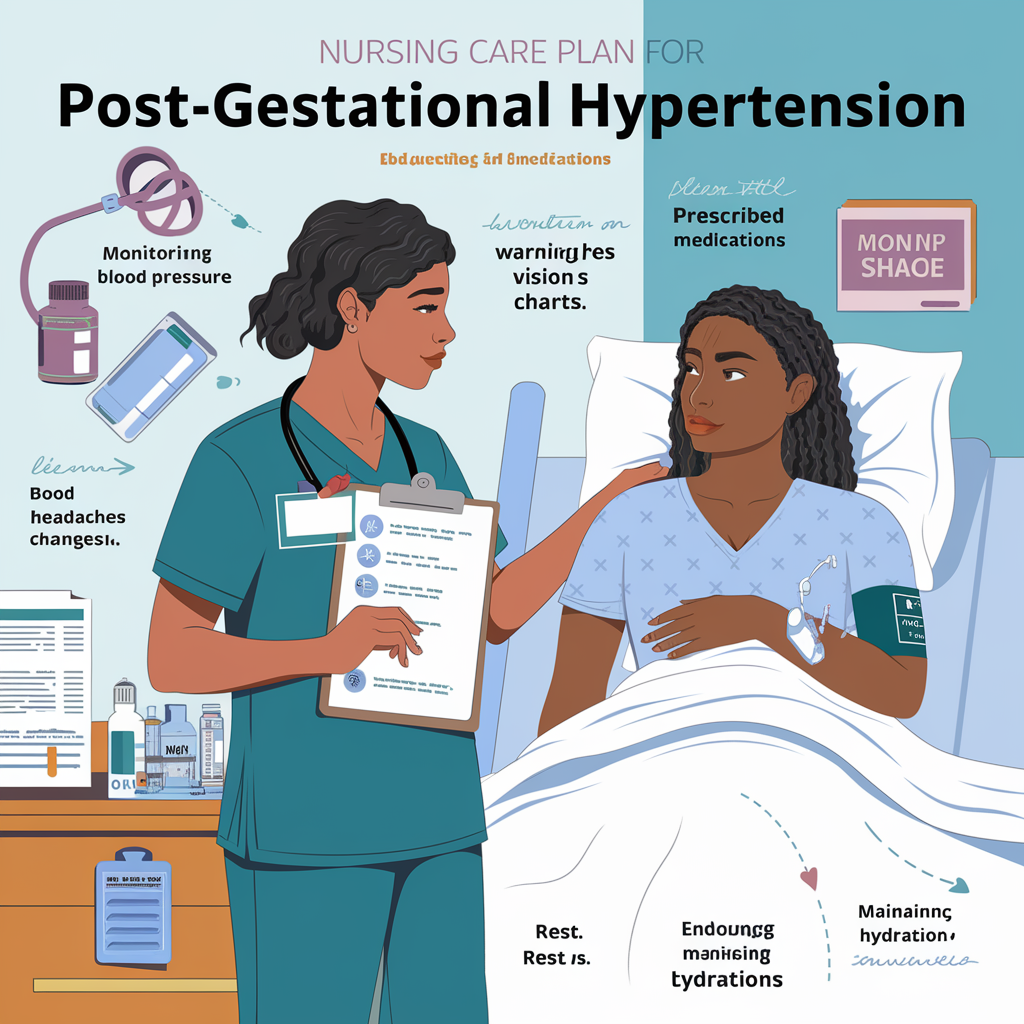
Nursing Interventions and Rationales:
1. Monitor Vital Signs Frequently
- Rationale: Monitoring Priya’s blood pressure is critical to understanding whether her condition is worsening. High blood pressure during pregnancy can lead to serious complications, so you’ll want to keep an eye on those numbers regularly.
2. Assess for Symptoms of Severe Hypertension and Preeclampsia
- Rationale: You’ll want to check for visual disturbances, headaches, or sudden swelling, all of which could signal preeclampsia or worsening gestational hypertension. These signs are red flags that need immediate attention!
3. Administer Antihypertensive Medications as Ordered
- Rationale: Medications like Methyldopa or Labetalol are commonly used to manage high blood pressure during pregnancy. This will help keep Priya’s blood pressure within a safer range and prevent complications for her and her baby.
4. Educate on Rest and Fluid Intake
- Rationale: Encourage Priya to get plenty of rest and reduce stress as much as possible. Proper hydration is key to reducing the swelling she’s experiencing, and rest will help lower her blood pressure.
5. Provide Emotional Support
- Rationale: A diagnosis of gestational hypertension can be stressful. Be there for Priya and offer emotional support. A calm, reassuring presence can help reduce anxiety and stress, which can exacerbate high blood pressure.
Nursing Goals:
- Goal 1: Priya will maintain a blood pressure less than 140/90 mmHg with the help of medication, lifestyle changes, and monitoring.
- Goal 2: Priya will report a reduction in headache intensity and swelling within the next 48 hours.
- Goal 3: Priya will demonstrate an understanding of gestational hypertension management by the end of the week.
Evaluation and Expected Outcomes:
- Priya’s blood pressure is consistently within normal range over the next 48 hours, showing an effective response to medications and interventions.
- Reduction in swelling and headache intensity: Priya reports significant improvement after a few days of following the care plan.
- Priya can confidently explain the signs and symptoms of gestational hypertension and know how to manage it with her healthcare provider’s guidance.
Conclusion
Creating an effective Gestational Hypertension NCP isn’t just about monitoring vital signs—it’s about keeping both the mother and baby safe, preventing complications, and supporting the patient emotionally and physically through a challenging time. With a strong understanding of nursing interventions, patient education, and ongoing monitoring, you can make a real difference in the lives of your patients dealing with this condition.
As a nursing student, you’ll need to be thorough, compassionate, and detail-oriented—and now, you’ve got the tools to do just that! Keep practicing, keep refining, and soon you’ll be a master at making comprehensive nursing care plans for any condition. 💪
FAQs About Gestational Hypertension NCP
- What is the difference between gestational hypertension and preeclampsia?
Gestational hypertension is high blood pressure that develops during pregnancy, while preeclampsia involves hypertension along with protein in the urine and organ dysfunction. Both are serious but different conditions. - What are the primary risk factors for gestational hypertension?
Obesity, a family history of hypertension, carrying twins or multiples, and previous hypertension during pregnancy are all common risk factors. - Can gestational hypertension affect the baby?
Yes, if left unmanaged, it can lead to preterm birth, low birth weight, or placental abruption, which can be dangerous for both the mother and baby. - How often should I monitor blood pressure in a patient with gestational hypertension?
Blood pressure should be checked regularly—at least twice a day, and more frequently if the patient shows signs of worsening hypertension. - What medications are commonly prescribed for gestational hypertension?
Labetalol, Methyldopa, and Nifedipine are commonly prescribed to help control high blood pressure during pregnancy.
Recommended Resources:
- Gestational Hypertension Guidelines – National Institute of Health (NIH)
- Pregnancy Hypertension Care Plan – American Pregnancy Association
- Nursing Care Plans for Hypertension – Nursing Times
This article will help you craft a solid NCP for gestational hypertension that addresses the most important aspects of patient care while ensuring the health of both the mother and the baby.


