Nephrotic Syndrome is a complex kidney disorder that requires careful monitoring and management. It is characterized by high proteinuria, edema formation, and low serum albumin levels, which can significantly affect a patient’s overall health. Proper nursing care is essential to prevent complications such as infections, thromboembolism, and malnutrition. This nursing care plan provides a step-by-step approach to assessment, diagnosis, and interventions. By following structured nursing strategies, healthcare professionals in India and globally can ensure patients receive holistic care, achieve optimal recovery, and maintain quality of life while living with nephrotic syndrome.

Assessment and Early Detection
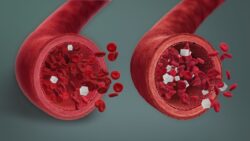
The first step in managing nephrotic syndrome is thorough patient assessment. Nurses should monitor urine output patterns, protein levels in urine, and vital signs such as blood pressure and heart rate. Assessing edema severity—including periorbital, pedal, and abdominal swelling—is crucial for early intervention. Regularly check laboratory values including serum albumin, cholesterol, and renal function tests. Nursing observations should also include dietary intake, weight changes, and signs of fluid overload. Proper documentation of these findings ensures timely communication with the medical team, allowing for individualized interventions and effective monitoring of disease progression.
Planning Nursing Interventions
Once the assessment is complete, nurses should develop a detailed care plan tailored to the patient’s needs. Interventions may include fluid management strategies, such as restricting sodium intake and monitoring fluid balance. Administer medications like diuretics and corticosteroids as prescribed, ensuring patients are educated on potential side effects. Implement skin care measures to prevent breakdown from edema and maintain mobility to reduce the risk of thromboembolism. Nutritional support is vital; plan a high-protein, low-sodium diet to help restore protein levels while preventing fluid retention. Education on self-monitoring for swelling, weight gain, and signs of infection empowers patients and caregivers.
Evaluation and Outcome Goals
Evaluating the effectiveness of nursing interventions involves monitoring clinical and laboratory improvements. Key goals include reducing edema levels, maintaining optimal serum albumin, and achieving stable body weight. Nurses should assess patient adherence to medication regimens and dietary recommendations. Improvement in urine protein levels and stable blood pressure indicate positive outcomes. Regular follow-ups and patient education reinforce long-term disease management. Documentation of progress allows the healthcare team to adjust the care plan as needed, ensuring patients with nephrotic syndrome experience fewer complications and a better quality of life.
Patient Education and Support
Education plays a crucial role in the management of nephrotic syndrome. Nurses should provide guidance on dietary modifications, proper medication adherence, and recognizing early warning signs of infection or relapse. Encourage patients and families to monitor daily weight, track urine output, and report sudden swelling. Emotional support and counseling can help manage anxiety and stress related to chronic illness. Collaborative care involving nephrologists, dietitians, and social workers enhances holistic support, enabling patients to actively participate in their recovery and maintain independence while effectively managing their condition.
| Assessment Parameter | Nursing Action | Frequency |
|---|---|---|
| Edema | Measure weight, observe swelling | Daily |
| Urine Protein | Collect 24-hour urine sample | Weekly |
| Serum Albumin | Check blood levels | Biweekly |
| Blood Pressure | Monitor and document | Every shift |
| Fluid Intake | Track oral and IV fluids | Continuous |
FAQs
1. What is nephrotic syndrome?
It is a kidney disorder causing protein loss and swelling.
2. How is edema managed in patients?
Through fluid restriction, diuretics, and daily weight monitoring.
3. Which diet is recommended?
A high-protein, low-sodium diet supports recovery and reduces swelling.
4. Why is patient education important?
It helps prevent complications and promotes self-care adherence.