Acute gastroenteritis is an inflammation of the stomach and intestines that causes symptoms such as diarrhea, vomiting, and abdominal pain. Nurses play a vital role in managing these patients with a structured approach. A clear nursing care plan for acute gastroenteritis and a precise nursing diagnosis for acute gastroenteritis guide healthcare professionals in delivering effective, timely care. This article provides essential tips, practical examples, and a sample care plan to help nurses improve patient outcomes.
Thank you for reading this post, don't forget to subscribe!
1. Introduction
Acute gastroenteritis causes inflammation in the stomach and intestines. It leads to fluid loss, electrolyte imbalances, and discomfort. A detailed nursing care plan for acute gastroenteritis enables nurses to structure their assessments, diagnoses, interventions, and evaluations. This plan also includes a nursing diagnosis for acute gastroenteritis that pinpoints key problems such as dehydration and pain. By following clear guidelines, nurses can manage symptoms, reduce complications, and support patient recovery.


2. Understanding Acute Gastroenteritis
Acute gastroenteritis is commonly caused by infections from viruses, bacteria, or parasites. The condition disrupts the digestive system and results in symptoms like:
- Diarrhea: Frequent, loose stools that lead to dehydration.
- Vomiting: Rapid loss of stomach contents, increasing the risk of dehydration.
- Abdominal Pain: Cramps and discomfort due to intestinal inflammation.
- Fever: An immune response to infection.
The severity of symptoms can vary. Early intervention helps prevent dehydration and other complications. Nurses must assess each patient carefully by monitoring vital signs, fluid intake, and laboratory results. A timely response is essential to stabilize the patient.
3. Nursing Diagnosis for Acute Gastroenteritis
A correct nursing diagnosis for acute gastroenteritis forms the foundation for targeted interventions. Common nursing diagnoses include:
- Deficient Fluid Volume:
Caused by excessive loss of fluids through diarrhea and vomiting. Signs include dry mucous membranes, decreased skin turgor, rapid pulse, and low blood pressure. - Risk for Electrolyte Imbalance:
Results from the loss of sodium, potassium, and other electrolytes. Patients may show muscle cramps, weakness, or cardiac irregularities. - Acute Pain:
Abdominal cramps and discomfort lead to pain that must be managed effectively. - Impaired Oral Mucous Membrane:
Vomiting can cause irritation and inflammation of the mouth and throat. - Risk for Infection:
The infectious nature of the cause requires strict adherence to infection control practices.
These diagnoses help nurses develop specific care strategies that address both the symptoms and underlying issues.
4. Developing a Nursing Care Plan for Acute Gastroenteritis
A nursing care plan for acute gastroenteritis is structured into five key steps:
- Assessment:
Gather data on patient history, symptoms, and laboratory values. Monitor vital signs and fluid balance. Look for signs of dehydration and electrolyte imbalances. - Nursing Diagnosis:
Use established guidelines to define issues such as deficient fluid volume and acute pain. A precise diagnosis directs the subsequent interventions. - Planning:
Set clear, measurable goals. For example, aim to stabilize vital signs within four hours and restore hydration within 24 hours. Goals should be short-term and long-term. - Intervention:
Execute targeted actions such as fluid replacement (oral or IV), electrolyte management, pain relief, and nutritional support. Nurses must also enforce infection control practices and educate patients. - Evaluation:
Regularly review patient progress. Adjust the care plan based on changes in vital signs, laboratory results, and patient feedback.
This structured approach ensures that each aspect of patient care is addressed, from symptom management to long-term recovery.
5. Key Nursing Interventions and Management
Effective management of acute gastroenteritis involves several critical interventions:
- Fluid and Electrolyte Replacement:
Administer IV or oral rehydration solutions as prescribed. Monitor intake and output to ensure proper hydration. Replace electrolytes to restore balance. - Vital Signs Monitoring:
Regularly check temperature, pulse, blood pressure, and respiratory rate. Early detection of changes prevents complications such as shock. - Pain Management:
Assess abdominal pain using a standardized scale. Administer analgesics according to the prescribed regimen. Use non-pharmacological methods like warm compresses for additional comfort. - Nutritional Support:
Provide small, frequent meals that are gentle on the stomach. Encourage a bland diet until symptoms improve. Educate the patient on avoiding irritants. - Infection Control:
Use hand hygiene, personal protective equipment (PPE), and isolation protocols to prevent the spread of infection. Teach patients and families proper infection prevention techniques. - Patient Education:
Instruct patients on the importance of hydration, recognizing symptoms of dehydration, and when to seek help. Clear education improves adherence and outcomes.
These interventions address both immediate symptoms and long-term recovery needs. They empower nurses to provide comprehensive care for patients with acute gastroenteritis.
6. Sample Nursing Care Plan
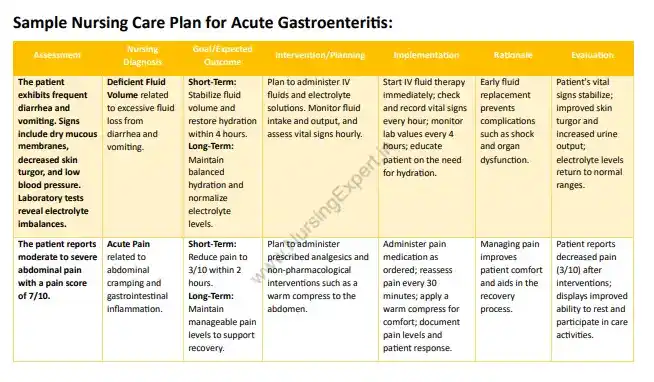
Below is a sample 7‑column nursing care plan for a patient with acute gastroenteritis. This plan illustrates each step from assessment to evaluation.
Sample Nursing Care Plan for Acute Gastroenteritis
| Assessment | Nursing Diagnosis | Goal/Expected Outcome | Intervention/Planning | Implementation | Rationale | Evaluation |
|---|---|---|---|---|---|---|
| The patient exhibits frequent diarrhea and vomiting. Signs include dry mucous membranes, decreased skin turgor, and low blood pressure. Laboratory tests reveal electrolyte imbalances. | Deficient Fluid Volume related to excessive fluid loss from diarrhea and vomiting. | Short-Term: Stabilize fluid volume and restore hydration within 4 hours. Long-Term: Maintain balanced hydration and normalize electrolyte levels. | Plan to administer IV fluids and electrolyte solutions. Monitor fluid intake and output, and assess vital signs hourly. | Start IV fluid therapy immediately; check and record vital signs every hour; monitor lab values every 4 hours; educate patient on the need for hydration. | Early fluid replacement prevents complications such as shock and organ dysfunction. | Patient’s vital signs stabilize; improved skin turgor and increased urine output; electrolyte levels return to normal ranges. |
| The patient reports moderate to severe abdominal pain with a pain score of 7/10. | Acute Pain related to abdominal cramping and gastrointestinal inflammation. | Short-Term: Reduce pain to 3/10 within 2 hours. Long-Term: Maintain manageable pain levels to support recovery. | Plan to administer prescribed analgesics and non-pharmacological interventions such as a warm compress to the abdomen. | Administer pain medication as ordered; reassess pain every 30 minutes; apply a warm compress for comfort; document pain levels and patient response. | Managing pain improves patient comfort and aids in the recovery process. | Patient reports decreased pain (3/10) after interventions; displays improved ability to rest and participate in care activities. |
This sample care plan offers a clear framework. You can modify the plan according to patient needs and clinical settings.
7. NURSING CARE PLAN FOR ACUTE GASTROENTERITIS PDF DOWNLOAD
Access our comprehensive Nursing Care Plan for Acute Gastroenteritis PDF Download to enhance your clinical practice. This detailed resource offers step-by-step guidelines on nursing diagnosis, intervention, and evaluation for managing acute gastroenteritis. The PDF includes practical examples, evidence-based strategies, and clear instructions to help you stabilize patients and improve outcomes. Download now to streamline your workflow and deliver consistent, high-quality care.
8. Patient and Family Education
Education is a critical component of a successful care plan. Nurses should educate patients and their families on the following:
- Understanding the Condition:
Explain what acute gastroenteritis is, its causes, and its symptoms. Use simple language to describe the impact on the digestive system. - Hydration and Nutrition:
Stress the importance of staying hydrated. Recommend oral rehydration solutions and a bland diet. Provide guidelines on safe food choices during recovery. - Medication Adherence:
Instruct patients on how to take medications properly. Explain the purpose of each medication and the importance of following the prescribed regimen. - Infection Prevention:
Teach proper handwashing techniques and the use of personal protective equipment. Advise on ways to reduce the spread of infection at home. - Symptom Monitoring:
Educate patients on how to recognize worsening symptoms, such as increased frequency of diarrhea, high fever, or signs of dehydration. Explain when to seek medical help.
Clear education fosters confidence and encourages proactive participation in the recovery process.
9. Frequently Asked Questions (FAQs)
- What is acute gastroenteritis?
Acute gastroenteritis is an inflammation of the stomach and intestines, often caused by viral, bacterial, or parasitic infections, which leads to symptoms such as diarrhea, vomiting, and abdominal pain. - Why is a nursing care plan important for acute gastroenteritis?
A nursing care plan standardizes patient care by outlining clear assessments, diagnoses, interventions, and evaluations. This structured approach helps prevent complications and supports recovery. - What are common nursing diagnoses for acute gastroenteritis?
Common diagnoses include deficient fluid volume, risk for electrolyte imbalance, acute pain, impaired oral mucous membrane, and risk for infection. - How do nurses manage dehydration in gastroenteritis patients?
Nurses administer fluids (IV or oral), monitor fluid intake and output, and regularly check vital signs and laboratory values to ensure proper hydration. - What role does patient education play in managing acute gastroenteritis?
Patient education helps individuals understand their condition, adhere to treatment plans, maintain proper nutrition and hydration, and recognize when to seek further care.
10. Conclusion
A comprehensive nursing care plan for acute gastroenteritis and an accurate nursing diagnosis for acute gastroenteritis are crucial in managing this condition effectively. Nurses who use structured plans can stabilize patients, prevent complications, and promote a speedy recovery. Clear assessments, targeted interventions, and patient education are key to achieving positive outcomes.
11. References and Sources
- Centers for Disease Control and Prevention. Gastroenteritis. Retrieved from https://www.cdc.gov/ncezid/acute-gastroenteritis/
- MedlinePlus. Diarrhea. Retrieved from https://medlineplus.gov/diarrhea.html
- American Academy of Pediatrics. Management of Gastroenteritis in Children. Retrieved from https://www.aap.org/en/patient-care/


