Introduction to Nursing Care Plans for Knee Pain
Knee pain is a common clinical presentation affecting diverse patient populations, from athletes with acute injuries to older adults managing chronic osteoarthritis. As nursing professionals, developing a structured nursing care plan for knee pain is critical to addressing pain, restoring function, and preventing complications. This guide provides a systematic, evidence-based approach to crafting care plans that align with best practices and prioritize patient-centered care.
Thank you for reading this post, don't forget to subscribe!
Step 1: Conducting a Thorough Assessment of Knee Pain
A robust nursing care plan for knee pain begins with a holistic assessment to identify underlying causes, severity, and functional limitations.
Patient History: Gathering Subjective Data
- Onset and Duration: Determine whether the pain is acute (e.g., post-injury) or chronic (e.g., degenerative joint disease).
- Pain Characteristics: Use the PQRST framework:
- Provocation/Palliation: What aggravates (e.g., weight-bearing) or alleviates (e.g., rest) the pain?
- Quality: Is the pain sharp, throbbing, or burning?
- Region/Radiation: Is the pain localized or radiating to adjacent areas?
- Severity: Utilize a 0–10 pain scale for objective measurement.
- Timing: Does the pain worsen at night or after activity?
- Medical and Surgical History: Screen for conditions like rheumatoid arthritis, prior surgeries, or trauma.
Physical Examination: Objective Findings
- Inspection: Assess for visible deformities, swelling, erythema, or bruising.
- Palpation: Check for warmth, tenderness, effusion, or crepitus.
- Range of Motion (ROM): Evaluate active and passive ROM limitations.
- Functional Assessment: Observe gait patterns, weight-bearing ability, and use of assistive devices.
Diagnostic Tools
- Imaging (X-ray, MRI) and lab tests (C-reactive protein, ESR) may be ordered to confirm diagnoses like fractures or infections.
Key Takeaway: A meticulous assessment ensures individualized care and avoids a “one-size-fits-all” approach.
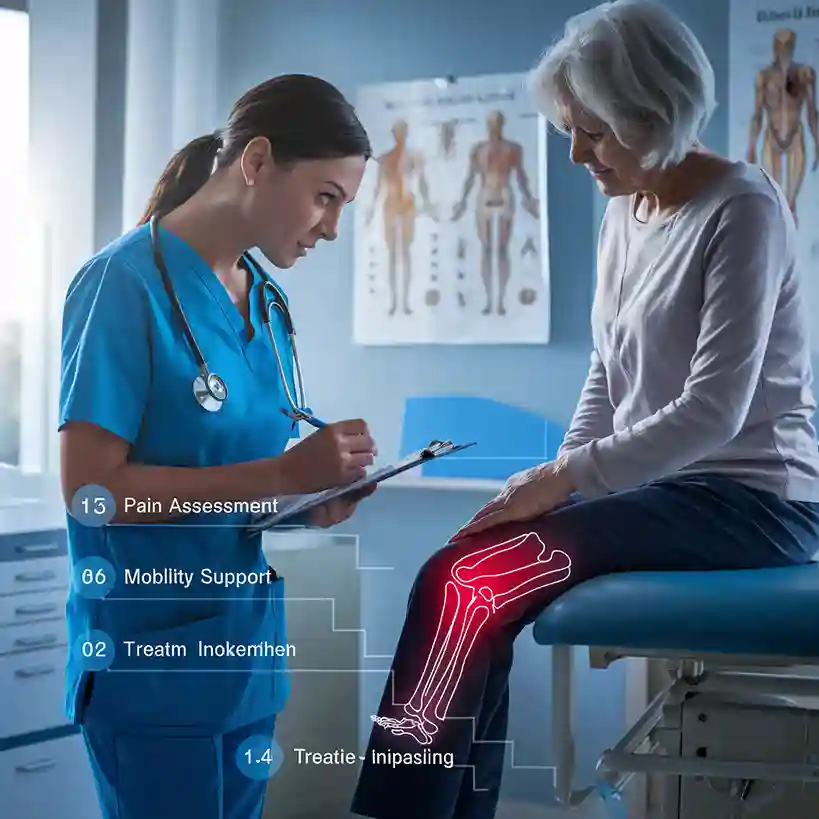
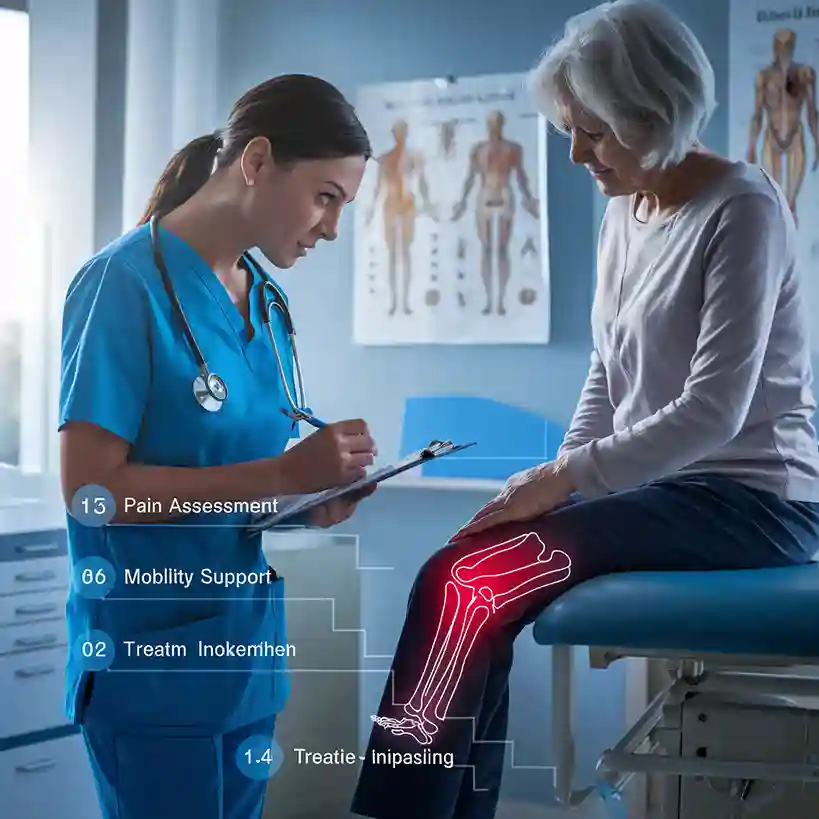
Step 2: Formulating Accurate Nursing Diagnoses
Nursing diagnoses bridge assessment findings to targeted interventions. Common diagnoses for knee pain management include:
- Acute Pain related to inflammation or tissue injury, as evidenced by verbal reports (e.g., “pain rated 8/10”) or guarding behaviors.
- Impaired Physical Mobility related to pain and joint stiffness, evidenced by reluctance to ambulate or limited ROM.
- Risk for Falls related to instability, muscle weakness, or altered balance.
Clinical Tip: Prioritize diagnoses based on immediacy of risk (e.g., falls prevention takes precedence in elderly patients).
Step 3: Establishing SMART Goals
Goals should be Specific, Measurable, Achievable, Relevant, and Time-bound:
- Short-Term Goal: “Patient will report pain reduction from 7/10 to ≤4/10 within 48 hours using prescribed analgesics and cold therapy.”
- Long-Term Goal: “Patient will achieve 90% ROM and ambulate independently for 100 meters within 4 weeks.”
Rationale: Clear goals provide direction for interventions and benchmarks for evaluation.
Step 4: Implementing Evidence-Based Interventions
Interventions must be tailored to the patient’s unique needs, preferences, and clinical context.
Pharmacological Interventions
- NSAIDs (e.g., Ibuprofen): Reduce inflammation and moderate pain. Monitor for GI upset or renal impairment.
- Acetaminophen: Suitable for mild pain or patients with NSAID contraindications.
- Opioids (e.g., Tramadol): Reserved for severe acute pain (e.g., post-surgery) with close monitoring for dependency.
Non-Pharmacological Interventions
- Cold Therapy: Apply ice packs for 15–20 minutes during the acute phase (first 48 hours) to minimize swelling.
- Heat Therapy: Use warm compresses for chronic stiffness to enhance blood flow.
- Elevation and Rest: Encourage limb elevation above heart level to reduce edema.
- Physical Therapy: Collaborate with PTs to design exercises (e.g., quadriceps strengthening, heel slides).
Fall Prevention Strategies
- Environmental Modifications: Remove tripping hazards, install grab bars, and ensure adequate lighting.
- Assistive Devices: Train patients in safe use of canes, walkers, or knee braces.
- Balance Training: Incorporate low-impact activities like Tai Chi for elderly patients.
Patient Education
- Activity Modification: Teach joint protection techniques (e.g., avoiding prolonged kneeling).
- Weight Management: Provide dietary counseling to reduce mechanical stress on knees.
- Medication Adherence: Explain dosing schedules and potential side effects.
Clinical Insight: Interventions should empower patients to actively participate in their recovery.
Step 5: Evaluating Outcomes and Refining the Care Plan
Continuous evaluation ensures the nursing care plan for knee pain remains effective and adaptive.
Pain Management Evaluation
- Reassess pain scores daily.
- Adjust analgesics if pain persists or side effects arise (e.g., NSAID-induced gastritis).
Mobility and Functional Progress
- Measure ROM weekly using a goniometer.
- Track ambulation distance and speed.
Fall Risk Reassessment
- Conduct timed “Up and Go” tests to assess balance improvements.
Patient Compliance
- Review exercise logs and conduct follow-up interviews.
Pro Tip: Involve patients in evaluation discussions to foster accountability.
Interdisciplinary Collaboration in Knee Pain Management
- Physical Therapists: Guide rehabilitation exercises and gait training.
- Orthopedic Specialists: Consult for surgical evaluations (e.g., arthroscopy, joint replacement).
- Dietitians: Address obesity-related joint stress through personalized meal plans.
Case Study: Applying the Nursing Care Plan Framework
Patient Profile: A 65-year-old female with osteoarthritis-related knee pain, BMI 32, reports pain at 7/10 worsened by stair climbing.
Care Plan Highlights:
- Interventions: Paracetamol 500mg TID, referral to PT for hydrotherapy, weight loss counseling.
- Outcome: Pain reduced to 3/10, 10% weight loss, and improved stair navigation in 8 weeks.
5 Essential FAQs for Nursing Students
- Q: How do I differentiate between acute and chronic knee pain in assessments?
A: Acute pain often follows trauma and has a sudden onset; chronic pain persists beyond 3–6 months and is linked to degenerative conditions. - Q: What non-pharmacological methods are effective for opioid-naïve patients?
A: Transcutaneous electrical nerve stimulation (TENS), acupuncture, and mindfulness-based stress reduction. - Q: How can I improve adherence to home exercise programs?
A: Provide written instructions, video demonstrations, and schedule follow-up calls. - Q: What are red flags indicating urgent referral to a specialist?
A: Sudden severe swelling, fever, or inability to bear weight (may indicate septic arthritis or fracture). - Q: How do cultural factors influence knee pain management?
A: Address language barriers, cultural beliefs about pain expression, and preferences for traditional therapies.
Recommended Resources for Evidence-Based Practice
- Clinical Guidelines:
- Textbooks:
- Nursing Care Plans: Diagnoses, Interventions, and Outcomes by Meg Gulanick & Judith L. Myers.
- Orthopedic Nursing: Core Curriculum by CMSA.
- Online Tools:
Conclusion: Elevating Practice Through Structured Care Planning
Designing a nursing care plan for knee pain demands clinical expertise, critical thinking, and empathy. By integrating thorough assessments, evidence-based interventions, and patient education, nurses play a pivotal role in enhancing quality of life for individuals with knee pain. As you refine your skills, remember that every care plan is a dynamic tool—responsive to patient progress and evolving clinical needs.


