Mental health nursing has emerged as a cornerstone of modern healthcare by 2025, driven by escalating mental health challenges, innovative care delivery models, and a pressing need for skilled professionals. Psychiatric-mental health nurse practitioners (PMHNPs) are at the forefront, addressing gaps in access, embracing technological advancements, and advocating for equitable care. This article delves into the multifaceted role of mental health nursing, exploring its challenges, opportunities, and future trajectory in a world increasingly attuned to psychological well-being.
Thank you for reading this post, don't forget to subscribe!
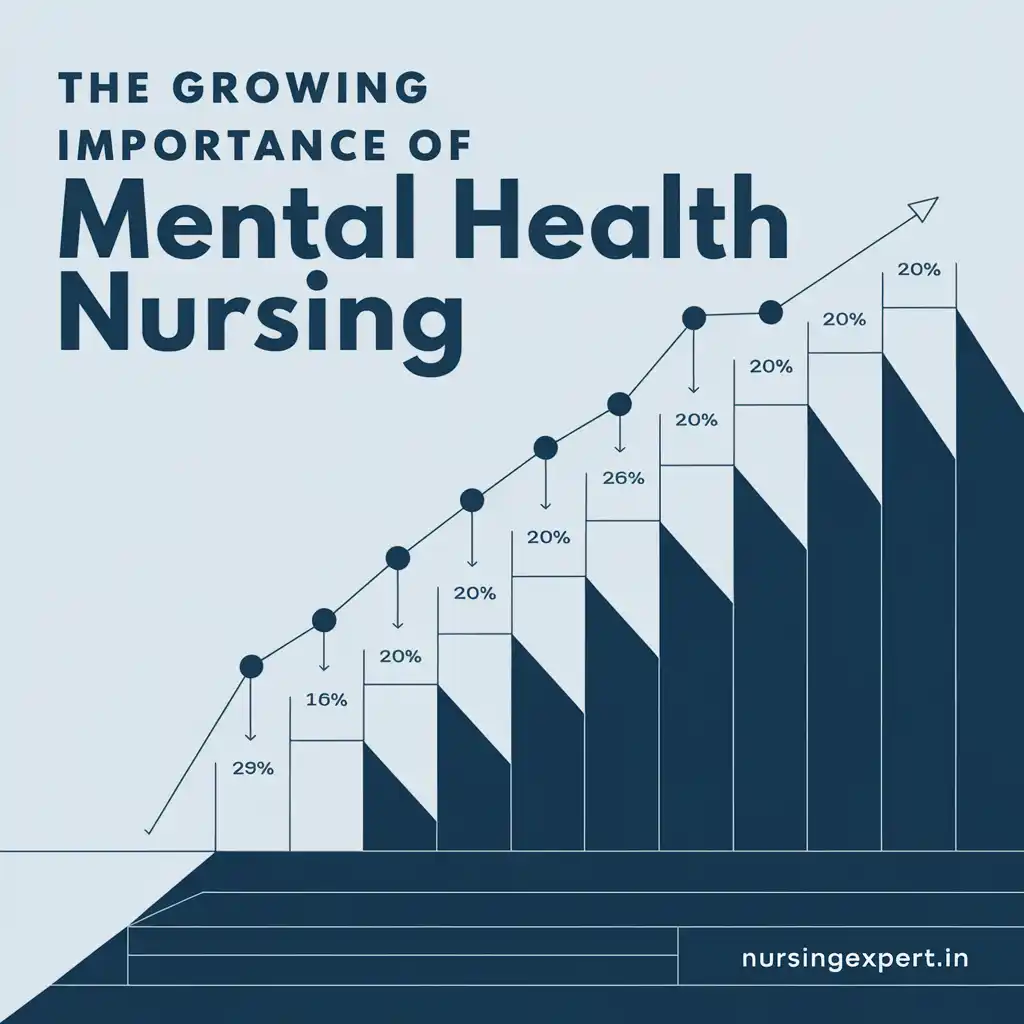
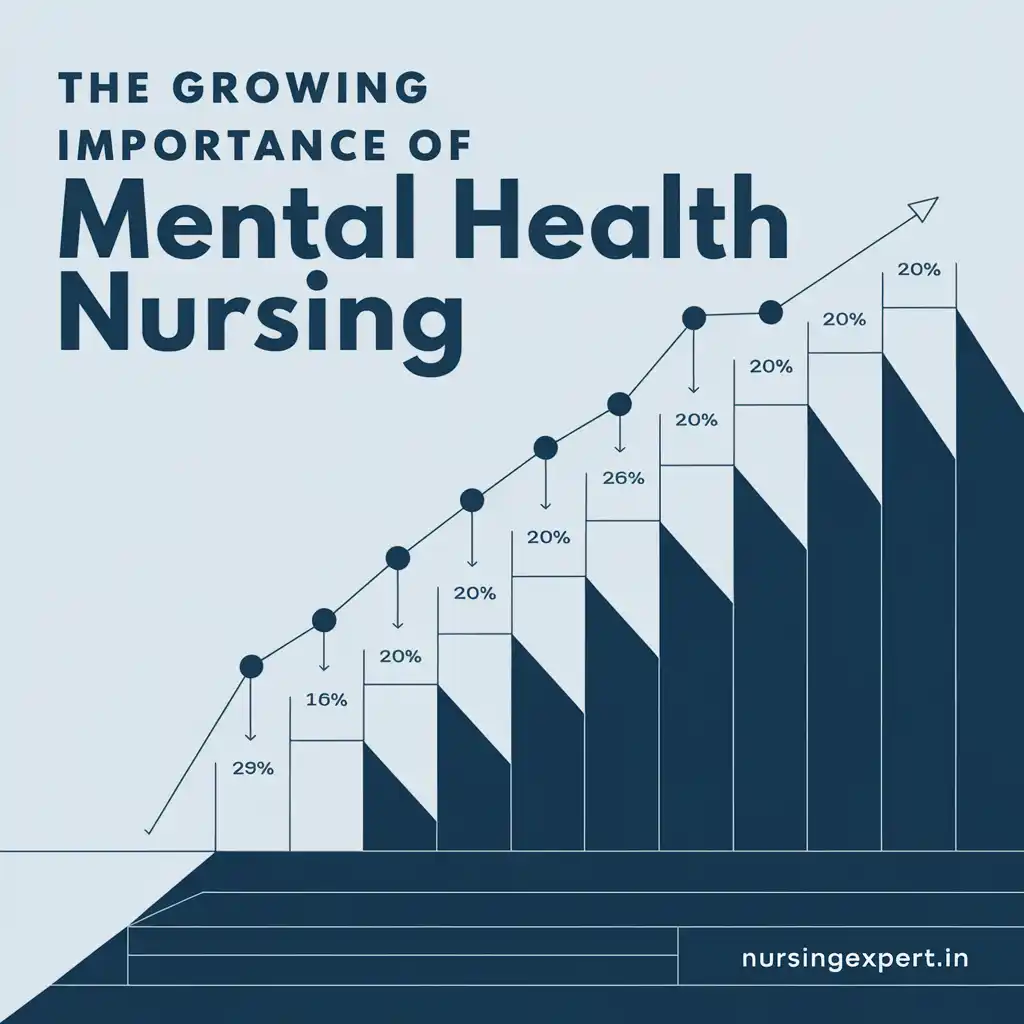
1. The Surging Need for Mental Health Services
A Global Mental Health Crisis
Mental health conditions have become a pervasive global issue. In the United States alone, one in five adults grapples with a mental health disorder annually. Depression stands out as the leading cause of disability worldwide, while anxiety disorders, substance use issues, and PTSD contribute to a mounting public health burden. The COVID-19 pandemic amplified this crisis, with the World Health Organization (WHO) reporting a 25% spike in anxiety and depression rates in its first year (WHO, 2022). This trend has strained healthcare systems, particularly in underserved regions.
Access Challenges
Access to mental health care remains a significant hurdle:
- 123 million Americans reside in areas designated as mental health professional shortage zones.
- 80% of rural counties lack a single psychiatrist, creating vast “mental health deserts.”
- Average wait times for appointments stretch beyond two months, pushing a 10% increase in emergency department visits for mental health emergencies.
Economic Implications
The economic fallout of untreated mental illness is profound. Experts estimate that by 2030, mental health disorders will drain the global economy of $16 trillion, largely due to reduced productivity and heightened healthcare costs (The Lancet Commission, 2018). PMHNPs play a vital role in mitigating this, delivering 60–70% of mental health care in underserved communities, particularly for Medicare and Medicaid patients who face the greatest barriers to treatment.
Case Study: Post-Pandemic Impact
Consider the lingering effects of the pandemic. A rural community in Montana saw a 30% rise in substance abuse cases post-2020, overwhelming its lone mental health clinic. A PMHNP, using telehealth, expanded services to include virtual counseling and medication management, reducing ED visits by 15% within six months. Such examples highlight the adaptability and impact of mental health nurses.
2. A Strained Workforce: Shortages and Retirement
The Numbers Tell the Story
The mental health nursing workforce is under immense pressure:
- Only 4–6% of registered nurses (RNs) specialize in psychiatric care.
- 27% of PMHNPs are expected to retire by 2030, shrinking an already limited pool.
- Nursing education often lacks robust mental health training, leaving many graduates hesitant to enter the field.
Root Causes
Several factors fuel this shortage. Stigma surrounding mental health care discourages some nurses from pursuing this path, while traditional curricula emphasize physical health over psychological care. Additionally, the emotional demands of the specialty can deter potential candidates, who may perceive it as more challenging than other nursing fields.
Building Capacity
Efforts to bolster the workforce are underway. Since 2012, universities have launched over 100 new PMHNP programs, producing more than 13,000 graduates. Dual-certification tracks, combining mental health with specialties like family practice, are also on the rise, equipping nurses to address the intertwined physical and mental needs of patients. For instance, Johns Hopkins School of Nursing has introduced a program blending psychiatric and primary care training, preparing nurses for holistic care delivery.
Retention Strategies
Retaining experienced PMHNPs is equally critical. Mentorship programs pairing retiring nurses with novices could preserve expertise, while incentives like loan forgiveness might encourage younger professionals to commit to underserved areas.
3. Technology’s Role in Mental Health Care
Telehealth Takes Center Stage
Technology has revolutionized mental health nursing:
- 60% of patients favor telehealth for its accessibility and reduced stigma.
- Remote consultations save $19–121 per visit, easing financial burdens on patients and systems.
- PMHNPs employ AI tools, such as the Rothman Index, to monitor patient data and predict potential crises.
Beyond Telehealth
Innovations extend beyond virtual visits. Mobile apps allow patients to track mood swings and share updates with providers, fostering proactive care. Virtual reality (VR) therapies are gaining traction for treating phobias and PTSD, immersing patients in controlled environments to confront fears safely. For example, a 2024 pilot program in California used VR to help veterans manage PTSD, reporting a 40% reduction in symptom severity.
Challenges and Ethics
Yet, technology introduces complexities. Engaging patients remotely—especially those in acute distress—requires advanced skills, and managing crises like suicidal ideation demands rigorous protocols. Ethical concerns loom large:
- Data Privacy: Breaches in telehealth platforms could expose sensitive patient information.
- Algorithmic Bias: AI tools may misdiagnose if trained on unrepresentative data, disproportionately affecting minority groups.
Balancing innovation with integrity is key to ensuring technology enhances, rather than undermines, mental health care.
4. Policy and Education Driving Change
Legislative Support
Policymakers are stepping up:
- The 21st Century Cures Act allocates $1 billion to expand the mental health workforce, including PMHNP training.
- State initiatives, like California’s $2.2 billion Children and Youth Behavioral Health Initiative, fund recruitment and education.
Integrated Care Models
Blending mental health into primary care settings is proving effective. Hackensack Meridian Health’s hybrid clinics, offering same-day mental health consultations, have slashed ER visits by 50%. The Veterans Health Administration similarly integrates mental health into its primary care framework, reducing stigma and improving outcomes.
Educational Reform
The American Association of Colleges of Nursing (AACN) now requires all nursing programs to teach mental health competencies, such as assessing psychological distress and providing basic interventions. Simulation labs, where students practice handling psychiatric emergencies, are becoming standard, ensuring graduates are better prepared.
5. Equity and Social Determinants of Health
Disparities in Care
Mental health inequities are stark:
- Low-income individuals face three times higher rates of untreated mental illness.
- Rural areas, dubbed “mental health deserts,” rely heavily on PMHNPs using telehealth.
Social Factors
Social determinants—housing, education, and community safety—shape mental health outcomes. For instance, a 2020 study found that people experiencing homelessness are five times more likely to suffer from mental disorders (National Alliance to End Homelessness, 2020). PMHNPs often bridge these gaps by linking patients to resources like food banks or housing programs.
Trauma-Informed Care
Training in trauma-informed care equips PMHNPs to support marginalized populations. This approach prioritizes safety, trust, and empowerment, recognizing trauma’s pervasive impact. A PMHNP in Chicago, for example, implemented trauma-informed practices in a clinic serving refugees, improving patient trust and engagement by 25%.
Community Impact
Since 2021, Hackensack Meridian Health has screened 1.8 million patients for social needs, addressing barriers that exacerbate mental health issues. Such efforts underscore the broader role of mental health nurses as advocates for systemic change.
6. Career Prospects and Financial Rewards
Competitive Compensation
The demand for PMHNPs translates into strong earning potential:
- Salaries average $134,000–$165,000, with top earners in states like Oregon exceeding $200,000.
- Compared to Family Nurse Practitioners (averaging $115,000), PMHNPs command a premium due to their specialized skills.
Job Growth
Employment opportunities are booming, with a 60% increase in openings since 2014 and 118,600 new roles projected by 2035 (U.S. Bureau of Labor Statistics, 2023). Beyond clinical practice, PMHNPs can explore academia, policy advocacy, or private telehealth ventures.
A Diverse Field
The flexibility of mental health nursing appeals to many. A PMHNP in Texas, for instance, transitioned from hospital work to a virtual practice, doubling her patient reach while maintaining work-life balance.
7. Supporting Nurse Well-Being
Burnout Epidemic
Mental health nurses face unique stressors:
- 76% reported burnout during the pandemic, driven by heavy caseloads and emotional tolls.
- Vicarious trauma, from absorbing patients’ distress, compounds the challenge.
Innovative Solutions
Healthcare systems are responding:
- AI automation streamlines documentation, freeing nurses for patient interaction.
- Flexible schedules and “safe spaces” with counseling access help nurses recharge.
- Mindfulness programs, like an 8-week course trialed in Ohio, reduced stress by 20% among participants (Journal of Psychiatric and Mental Health Nursing, 2019).
Ethical Mandate
The American Nurses Association (ANA) now mandates self-care in its Code of Ethics, urging employers to provide wellness resources. Peer support networks further bolster resilience, offering a space to process shared experiences.
8. Charting the Future
Strategic Priorities
To sustain mental health nursing’s momentum, four areas demand focus:
- Education Expansion: Increase PMHNP programs and faculty development through partnerships with hospitals.
- Tech Integration: Scale telehealth and AI responsibly, ensuring privacy and equity.
- Policy Reform: Standardize licensure across states and align reimbursement with physical health services.
- Equity Focus: Invest in underserved regions via mobile clinics and community collaborations.
A Vision for 2025 and Beyond
Mental health nursing is poised to redefine healthcare. By blending clinical expertise with advocacy and innovation, PMHNPs are building a future where mental well-being is a universal priority.
Conclusion
In 2025, mental health nursing transcends traditional roles, serving as a lifeline for millions. PMHNPs bridge divides, champion justice, and harness technology to deliver transformative care. Their influence will only grow as societies recognize mental health’s integral role in overall wellness.
For those considering this path, mental health nursing offers purpose and opportunity. For leaders, investing in this workforce promises a healthier, more equitable future. As we move forward, PMHNPs will remain torchbearers in a healthcare revolution centered on the mind and soul.
Frequently Asked Questions (FAQs)
Q: What does a psychiatric-mental health nurse practitioner (PMHNP) do?
A: PMHNPs are advanced practice nurses who assess, diagnose, and treat mental health conditions. They prescribe medications, offer therapy, and coordinate care, often in underserved settings.
Q: How do I pursue a career as a PMHNP?
A: Start with a nursing degree (BSN), then earn a Master’s (MSN) or Doctorate (DNP) in psychiatric-mental health nursing. Pass the certification exam from the American Nurses Credentialing Center (ANCC) to practice.
Q: What obstacles do mental health nurses face?
A: They contend with shortages, burnout, and complex patient needs. Integrating technology and addressing social inequities add further challenges.
Q: How has technology changed mental health nursing?
A: Telehealth has broadened access, while AI and VR enhance treatment options. However, it requires managing privacy risks and ensuring patient engagement.
Q: What’s the employment outlook for PMHNPs?
A: Excellent—118,600 new jobs are expected by 2035, with salaries often topping other nursing fields due to high demand.
Q: Why is nurse well-being a priority?
A: Burnout affects care quality. Supporting nurses through flexible schedules and wellness programs ensures they thrive, benefiting patients.
References
- American Association of Colleges of Nursing. (2021). Essentials: Core Competencies for Professional Nursing Education.
- California Department of Health Care Services. (2022). Children and Youth Behavioral Health Initiative.
- Journal of Psychiatric and Mental Health Nursing. (2019). “The impact of mindfulness-based stress reduction on nurse burnout.”
- National Alliance to End Homelessness. (2020). Mental Health and Homelessness.
- The Lancet Commission on global mental health and sustainable development. (2018). The Lancet Commission on global mental health and sustainable development.
- U.S. Bureau of Labor Statistics. (2023). Occupational Outlook Handbook: Nurse Practitioners.
- World Health Organization. (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide.