Nursing Care Plan for Ventilator Patient: High-quality care for ventilator patients is key in ICU nursing. Nurses are vital in ensuring patients get the best care. A well-planned ventilator care plan is essential for this goal. Mechanical ventilation nursing requires a deep understanding of ventilator care principles and practices.
Thank you for reading this post, don't forget to subscribe!
This article will cover the importance of a ventilator care plan and how it improves patient outcomes. We’ll also explore mechanical ventilation nursing principles. Whether you’re an experienced nurse or new to ICU nursing, this article will help you master ventilator care and improve patient outcomes.
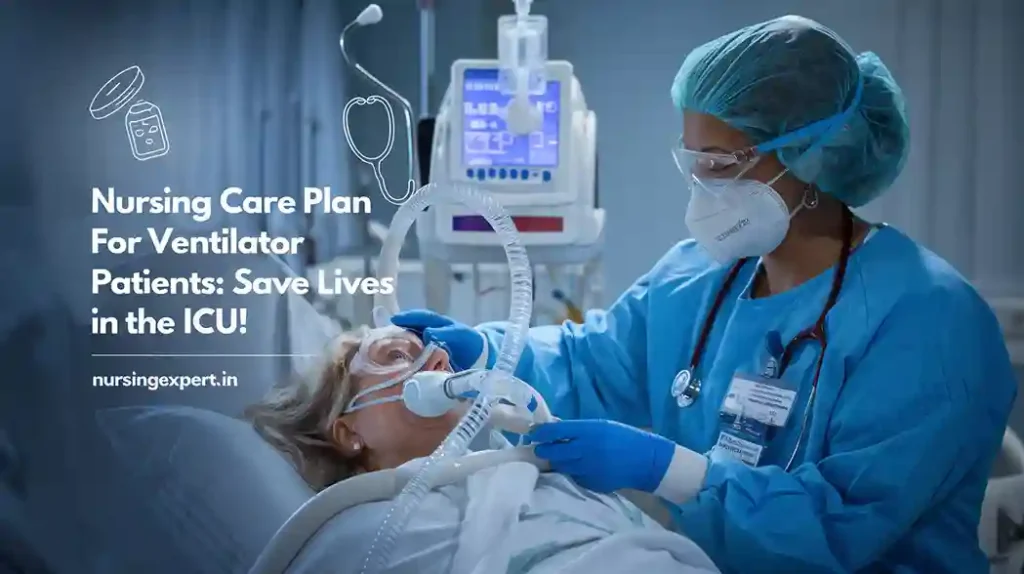
By the end of this article, you’ll understand ventilator care’s key aspects and how to create a detailed care plan. You’ll also learn about the latest in mechanical ventilation nursing. This knowledge will help you in real-world situations.
Key Takeaways
- Developing a detailed ventilator care plan is key to better patient outcomes in ICU nursing.
- Understanding mechanical ventilation nursing principles is critical for high-quality ventilator patient care.
- A well-planned ventilator care plan can lower complication risks and improve patient outcomes.
- Nurses are essential in ensuring patients receive the best care, needing a deep ventilator care understanding.
- Mastering ventilator care helps nurses improve patient outcomes and reduce complications in ICU nursing.
Understanding Mechanical Ventilation: Essential Principles for Nurses
High-quality icu nursing care starts with knowing mechanical ventilation. It’s a therapy for patients with breathing problems. Nurses use mechanical ventilators to help or take over breathing. This is key to stop ventilator-associated pneumonia (vap) prevention.
To do well in mechanical ventilation nursing, nurses need to know the basics. This includes the different modes and settings of ventilators. They also need to know the parts of the ventilator, like the circuit, humidifier, and oxygen sensor.
Basic Ventilator Modes and Settings
- Volume-controlled mode: delivers a set tidal volume with each breath
- Pressure-controlled mode: delivers a set inspiratory pressure with each breath
Key Components of Mechanical Ventilators
Knowing the parts of mechanical ventilators is key for icu nursing care. The circuit, humidifier, and oxygen sensor work together. They help give safe and effective breathing support.
Indications for Mechanical Ventilation
Mechanical ventilation is needed for patients with breathing failure. This includes ARDS, COPD, and pneumonia. Nurses should know when to use this therapy and how to check if a patient needs it.
Understanding mechanical ventilation is vital for icu nursing care. It helps prevent ventilator-associated pneumonia (vap) prevention. Nurses need to know the basics of ventilators and their parts to do their job well.
Initial Patient Assessment and Preparation
High-quality care for ventilator patients starts with a thorough assessment and preparation. This step checks the patient’s breathing, heart, and brain health. It’s key to figure out the best treatment plan. Good endotracheal tube care is vital to avoid problems and keep the airway safe.
In the ICU, icu nursing care teams are essential. They assess and prepare patients for mechanical ventilation. They use tools and techniques to check the patient’s condition and create a care plan. This plan might include helping the patient with the ventilator weaning process to recover and become independent again.
Important parts of patient assessment and preparation include:
- Evaluating the patient’s respiratory rate and oxygen saturation levels
- Assessing the patient’s cardiovascular status, including blood pressure and heart rate
- Checking the patient’s neurological status, including level of consciousness and cognitive function
Healthcare teams follow a structured approach for patient assessment and preparation. This ensures patients get the best care and outcomes. It includes top-notch icu nursing care and support for the ventilator weaning process to help patients recover and do well.
Comprehensive Nursing Care Plan for Ventilator Patient
A good care plan for ventilator patients needs a team effort. It includes sedation management, respiratory assessment nursing, and critical care interventions. Nurses focus on making patients comfortable, safe, and helping them get better. They assess needs, create care plans, and watch how patients do.
Important parts of a care plan are:
- Keeping the airway open and avoiding problems
- Setting up the ventilator right to help with breathing
- Watching the heart and blood pressure closely
Nurses use sedation management and respiratory assessment nursing to help patients. They also use critical care interventions like turning patients to help with breathing.
Creating a good care plan takes teamwork. Nurses, doctors, and others work together to help ventilator patients. By focusing on the patient and using the latest care methods, nurses can greatly improve patient care in the ICU.
Essential Ventilator Parameters and Monitoring
As a critical care nurse, it’s key to watch ventilator parameters closely. This ensures patients get the best care. We track vital signs and respiratory data like heart rate, blood pressure, and oxygen levels. ICU nursing care demands attention to detail and understanding complex data.
Managing ventilator alarms well is also vital for patient safety. We set alarm limits, respond to them, and fix issues. Nurses who stay alert and proactive offer top-notch care and better patient results.
Vital Signs and Respiratory Parameters
- Heart rate and blood pressure monitoring
- Oxygen saturation and respiratory rate monitoring
- Temperature and blood gas analysis
Nurses also need to be good at critical care interventions. This includes suctioning and giving meds. With skills in ventilator management, nurses give full care to ICU patients.
Preventing Ventilator-Associated Complications
Stopping ventilator-associated problems is key in icu nursing care. Ventilator-associated pneumonia (VAP) is a big issue. It can be stopped with proven methods. Vap prevention includes washing hands, oral care, and suctioning.
A detailed ventilator care plan is vital to avoid VAP and other issues. It involves checking the patient’s breathing and watching vital signs. A good ventilator care plan helps nurses lower VAP risk. This improves patient results and shortens ICU stays.
Some important vap prevention steps are:
- Proper hand hygiene before and after interacting with the patient
- Regular oral care to reduce the risk of bacterial colonization
- Effective suctioning techniques to remove secretions and prevent aspiration
By using these methods and sticking to a detailed ventilator care plan, nurses can give top-notch icu nursing care. This helps cut down on ventilator-related problems.
| Strategy | Description |
|---|---|
| Hand Hygiene | Proper hand hygiene before and after interacting with the patient |
| Oral Care | Regular oral care to reduce the risk of bacterial colonization |
| Suctioning Techniques | Effective suctioning techniques to remove secretions and prevent aspiration |
Evidence-Based Suctioning Techniques and Protocols
Proper care of endotracheal tubes is key to avoiding ventilator-associated pneumonia (vap) and ensuring top-notch ICU nursing care. Suctioning is a vital part of this care. It’s important to use evidence-based methods and protocols to avoid complications.
Regular suctioning keeps the airway clear, lowering the chance of vap and other breathing problems. It’s vital to stick to guidelines for suctioning frequency and to document it well. This ensures care is consistent and of high quality.
Closed vs. Open Suctioning Methods
Closed suctioning is usually the better choice because it lowers the risk of bacteria getting into the airway. But, open suctioning might be needed sometimes. It’s important to follow strict protocols to lessen the risk of problems.
Frequency and Documentation Guidelines
The frequency and guidelines for suctioning vary based on the patient’s health and the hospital’s rules. It’s key to follow these guidelines and document suctioning accurately. This helps keep care consistent and effective.
| Suctioning Method | Frequency | Documentation |
|---|---|---|
| Closed Suctioning | As needed, typically every 2-4 hours | Document suctioning procedure, including date, time, and amount of secretions removed |
| Open Suctioning | As needed, typically every 2-4 hours | Document suctioning procedure, including date, time, and amount of secretions removed |
By sticking to evidence-based suctioning methods and protocols, ICU nursing teams can lower the risk of vap and other issues. This ensures the best results for their patients.
Optimizing Patient Comfort and Sedation Management
Effective sedation management is key to top-notch care for ventilator patients. It means checking how comfortable the patient is and creating a sedation plan just for them. This helps lower anxiety, discomfort, and stress, making the patient’s experience better.
In respiratory assessment nursing, we must look at the patient’s whole health, including their breathing. Critical care interventions, like using a ventilator, need careful sedation to keep the patient safe and comfy.
Some important things to think about for better patient comfort and sedation include:
- Checking the patient’s pain and discomfort often
- Creating a sedation plan that fits the patient’s needs and medical history
- Keeping a close eye on the patient’s vital signs and breathing
By focusing on patient comfort and sedation, healthcare workers can make care better. This leads to better patient results, fewer problems, and higher care quality in the ICU.
Advanced Respiratory Assessment Skills
Respiratory assessment nursing is key in icu care. It helps spot issues early and act fast. Nurses use these skills to catch respiratory problems early and treat them right.
Some important parts of advanced respiratory assessment include:
- Chest assessment techniques, such as auscultation and percussion, to evaluate lung sounds and detect abnormalities
- Recognition of respiratory distress, including signs and symptoms such as tachypnea, dyspnea, and cyanosis
- Documentation requirements, including accurate and detailed recording of patient data and treatment plans
To be good at respiratory assessment, nurses need to know a lot about lungs and how they work. They must also be able to understand patient data and make smart choices. This helps them give the best care to patients with breathing problems.
Nurses can get better at respiratory assessment by learning more and staying current. This helps them give better care and improve patient results in icu settings.
| Skill | Description |
|---|---|
| Chest Assessment | Evaluation of lung sounds and detection of abnormalities |
| Respiratory Distress Recognition | Identification of signs and symptoms of respiratory distress |
| Documentation | Accurate and detailed recording of patient data and treatment plans |
Patient Positioning and Mobility Protocols
In icu nursing care, how patients are positioned is key to avoiding problems and helping them get better. A good ventilator care plan must include how to move and position patients. This helps prevent bed sores, improves breathing, and makes patients more comfortable.
Some important things to think about when positioning patients include:
- Proper alignment of the patient’s head, neck, and body
- Adequate support for the patient’s back and limbs
- Regular repositioning to prevent pressure ulcers and promote blood flow
Nurses can give top-notch icu nursing care by adding patient positioning and mobility to the ventilator care plan. Regular assessment and adjustment of patient positioning ensures patients get the best care.
Communication Strategies with Ventilated Patients
Effective communication is key in mechanical ventilation nursing. It ensures patients get the best care. A good ventilator care plan must include ways to talk with patients, families, and healthcare teams.
Non-verbal signs like gestures and facial expressions help share feelings and needs. It’s also vital to educate and support families in ventilator care plan. This way, they can be part of the patient’s care journey.
Non-verbal Communication Methods
- Use of pictures or diagrams to convey information
- Touch and physical contact to provide comfort
- Facial expressions to show empathy and understanding
Family Education and Support
Family members need to know about the patient’s health, treatment, and ventilator care plan. Regular updates, counseling, and support groups can help. Communication strategies should fit each family’s needs.
By using these methods in mechanical ventilation nursing, care teams can better patient outcomes. They can also make families happier and create a more caring environment.
Weaning Protocols and Assessment
The ventilator weaning process is a key part of caring for patients on ventilators. It needs careful planning and assessment to help them breathe on their own. Managing sedation is important to reduce pain and anxiety during this time. Nurses play a big role in checking if a patient is ready to start weaning and watching their progress.
Important parts of the ventilator weaning process include:
- Checking the patient’s breathing and overall health
- Creating a weaning plan that fits the patient’s needs and goals
- Using proven methods to help the patient breathe without the ventilator
Respiratory assessment nursing is key in spotting any problems and changing the weaning plan if needed. By combining sedation management and ventilator weaning process in the care plan, healthcare teams can help patients better and lower the chance of complications.
- Keep an eye on the patient’s breathing and adjust the weaning plan if necessary
- Teach the patient and their family about the weaning process
- Work with the team to solve any issues that come up during weaning
By using a clear method for ventilator weaning and focusing on respiratory assessment nursing, healthcare teams can make care in the ICU better and help patients more.
Emergency Response and Troubleshooting
In the ICU, ventilator alarm management is key for patient safety. Nurses must act fast and well in emergencies like ventilator failures or patient distress. They need skill, attention to detail, and quick thinking.
Common emergencies include patient disconnection, circuit blockages, and equipment breakdowns. In these cases, icu nursing care teams must find and fix the problem fast. This might mean calling a code blue or alerting the emergency team.
Good ventilator alarm management mixes technical skills, critical thinking, and teamwork. Nurses must understand alarms and work with the team to respond well. This focus on critical care interventions and icu nursing care helps avoid bad outcomes and improves patient care.
- Stay calm and assess the situation
- Activate rapid response protocols as needed
- Communicate with other members of the healthcare team
- Take corrective action to resolve the emergency
By following these steps and focusing on ventilator alarm management and icu nursing care, teams can give top-notch care to ventilator patients. This reduces the chance of bad events.
| Emergency | Response |
|---|---|
| Patient disconnection | Reconnect patient to ventilator, assess for distress |
| Ventilator circuit occlusion | Clear occlusion, assess for patient distress |
| Equipment failure | Activate backup equipment, notify maintenance team |
Documentation and Quality Improvement
Effective icu nursing care depends on detailed documentation and a solid ventilator care plan. This makes sure all patient care details are well-documented and easy for the healthcare team to access.
Important parts of documentation include:
- Accurate assessment and planning
- Implementation of the care plan
- Ongoing evaluation and adjustment of the plan as needed
By focusing on documentation and maintaining high-quality icu nursing care, healthcare professionals can greatly improve patient results. A well-organized ventilator care plan is key to achieving this goal.
In conclusion, combining detailed documentation with a thorough ventilator care plan is vital for top-notch icu nursing care. This approach helps healthcare teams provide the best care, leading to better health outcomes and a higher quality of life for patients.
Conclusion: Ensuring Excellence in Ventilator Patient Care
Providing top-notch ventilator care is key for ICU nurses. By learning about mechanical ventilation and using proven nursing care, we help our patients get the best care. This ensures they have a good chance of recovery.
Good care starts with watching over patients’ breathing closely. We must also manage their airways well and prevent problems before they start. Keeping your skills sharp and knowing the latest in ventilator care helps you give the best care possible.
Being a champion for patient safety and pushing for better care can change lives. Let’s work together to improve ventilator nursing. This way, we can save more lives in the ICU.
FAQ
What are the key priorities in airway management for ventilator patients?
For ventilator patients, keeping the airway open is key. Nurses must ensure the endotracheal tube is correctly placed and secured. They also need to prevent complications like pneumonia and regularly check the patient’s breathing.
How can nurses optimize ventilation and oxygenation goals for ventilator patients?
Nurses should watch the patient’s breathing closely. They need to adjust the ventilator settings as needed. Following evidence-based strategies to prevent complications is also important.
What are the essential ventilator parameters that nurses should monitor, and how can they interpret the data?
Nurses must monitor vital signs and breathing parameters. They should also check blood gas analysis. Being able to understand this data helps them make better care decisions.
How can nurses effectively prevent ventilator-associated pneumonia (VAP) in ICU patients?
To prevent VAP, nurses should follow strict hand hygiene and cuff pressure checks. Regular suctioning and oral care are also key. They must watch for signs of infection and act quickly.
What are the best practices for suctioning ventilator-dependent patients, and how can nurses minimize complications?
Nurses should use sterile technique and the right suction catheter size. They should limit suctioning time to avoid harm. Following protocols and documenting the process is important.
How can nurses improve oxygenation in ventilated patients, and what are the key nursing interventions?
Nurses can improve oxygenation by adjusting ventilator settings and positioning. Evidence-based interventions like prone positioning help too. They must monitor the patient’s breathing closely.
What are the steps to assess a ventilator-dependent patient’s readiness for weaning?
Nurses should check the patient’s breathing and heart stability. They must also consider the patient’s overall health. This assessment is critical and should involve the team.
What are the guidelines for oral care in intubated patients, and how can nurses ensure proper implementation?
Nurses should use soft-bristled toothbrushes and anti-microbial mouthwashes. Regular suctioning is also important. Following a standard oral care protocol helps prevent pneumonia.
How can nurses effectively communicate with a patient on mechanical ventilation, and what are the strategies for non-verbal communication?
Nurses can use gestures and writing to communicate. Engaging the patient and their family is key. Nurses should also reassure them and address their concerns.
What are the evidence-based sedation protocols for ventilated patients, and how can nurses optimize sedation management?
Nurses should use a sedation scale and follow guidelines for sedation. They play a big role in managing sedation and watching for side effects.
What is the role of mobility exercises in ventilator care, and how can nurses implement them effectively?
Mobility exercises are vital to prevent complications. Nurses should work with physical therapy and follow a mobility plan. Involving the patient and family is important.


